Online CE Programs

A Roundtable Discussion on Complement 3 Glomerulopathy (C3G): Improving Diagnosis, Risk Stratification, and Therapeutic Strategies
Complement 3 glomerulopathy (C3G) is a rare, progressive kidney disease characterized by dysregulation of the alternative pathway (AP) of the complement cascade, either due to genetic variants or acquired humoral factors1. About 50% of patients with C3G progress to kidney failure within 10 years of diagnosis2,6. Diagnosis and management are frequently delayed in part due to overlapping clinical presentations, histologic features, and underlying pathophysiologies.
This on-demand CME webinar will review illustrative patient cases, discussing consensus guideline treatment recommendations and the uncertainties, challenges, and considerations regarding the diagnosis and management of patients with C3G in clinical practice using an interactive roundtable conversation format.
Acromegaly: An Interactive Discussion with 3 Physician Experts
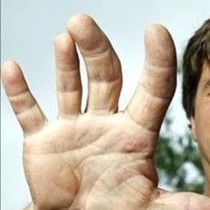
Acromegaly is a rare, chronic, progressive disease characterized by an excess secretion of growth hormone (GH) and increased circulating insulin-like growth factor 1 (IGF-1) concentrations. It is caused, in most cases, by pituitary adenomas that interfere with normal pituitary function. The clinical diagnosis, based on symptoms related to GH excess, is often delayed due to the gradual and subtle nature of the disease. Consequently, patients often have established systemic complications at diagnosis with increased morbidity and premature mortality.
Our three key opinion leaders who specialize in acromegaly will discuss three patient cases covering the consequences of a delayed diagnosis including strategies for a proper evaluation to avoid a misdiagnosis, address management strategies that can impact overall patient outcomes, and provide an in-depth look at the latest clinical evidence in the acromegaly treatment landscape.

Exploring Biosimilars in Pediatric Psoriasis: Emerging Treatment Options
Biosimilars are complex biologic therapies derived from living organisms and developed to be highly similar to an FDA-approved reference product in structure, function, and clinical performance, without clinically meaningful differences in safety, purity, or potency. This activity will review current advancements in the understanding and clinical application of biosimilars for the management of psoriasis. Growing evidence supports their safety, efficacy, and real-world integration, highlighting biosimilars as cost-effective alternatives to originator biologics and important tools for expanding patient access to high-quality biologic treatments.

Highlights from ACEP - Severe Abdominal Pain: Could it be an Acute Porphyria Attack?
Patients with certain inherited metabolic disorders often arrive in the ED with porphyria-like attacks. To better understand AHP (acute hepatic porphyria) whose main acute presentations include severe abdominal pain, extensive neuropathy issues, disabling respiratory symptoms, tachycardia, vomiting, and more, patient cases will be reviewed covering these neurovisceral acute attacks, with recommended strategies for immediate patient treatment will be discussed.

Highlights from the ASBMR: Clinical Phenotypes of ENPP1 Deficiency: GACI, ARHR2, and Beyond…
Generalized Arterial Calcification of Infancy (GACI) is a rare mineralization disorder caused by mutations in the ENPP1 or ABCC6 genes, affecting the circulatory system in addition to other body systems. Those individuals who survive into adulthood often have side effects of the disease, including Autosomal Recessive Hypophosphatemic Rickets Type 2 (ARHR2). Monoallelic Heterozygous ENPP1 Deficiency affects the ability to regulate calcium and phosphate levels leading to decreased inorganic pyrophosphate (PPi), and to increased calcium deposition in the vessel wall. Another clinical phenotype of ENPP1 Deficiency includes Ossification of the Posterior Longitudinal Ligament (OPLL), which may also be associated with hypophosphatemic rickets, and other skeletal conditions.
Highlights from the 2024 ASBMR satellite symposium will be offered soon as an on-demand webinar, where experts will review clinical phenotypes of ENPP1 deficiency including GACI, ARHR2, OPPL and others by providing guidance for treatment initiation, ending with a discussion of emerging treatment options, to enhance the clinician’s confidence in managing patients with these disorders.

Hypophosphatasia (HPP): Proposed HPP International Working Group Criteria
Hypophosphatasia (HPP) is a progressive, debilitating and sometimes fatal metabolic bone disease caused by loss of function mutations in the ALPL gene. Its clinical manifestations and severity of symptoms vary widely from patient to patient.
A multinational consortium of key opinion leaders, who are world specialists in hypophosphatasia (HPP), convened virtually during the past couple of years to recommend criteria for the diagnosis of HPP in children and adults, given that there are no formal diagnostic guidelines HPP.
Our two presenters are co-authors of the Proposed Criteria and will offer a review of the criteria including the measurable factors or parameters used to determine them, consensus recommendations for clinical practice, and appropriate treatment. By providing practical information and tools to help healthcare professionals better understand the diagnostic process, patients can be diagnosed earlier and experience better disease management and quality of life.

New Int'l Treatment Guidelines for X-Linked Hypophosphatemia: Improving Diagnosis + Management
X-linked hypophosphatemia (XLH) is the most common cause of inherited phosphate wasting and is associated with severe complications resulting from unresolved childhood symptoms, including disease progression. Diagnosis and specific treatment are frequently delayed leading to poorer patient outcomes.
This on-demand CME webinar will review the latest new global guidelines presented by three of the authors, including the Chair, based on GRADE methodology, and endorsed by several global organizations including the ASBMR and the Endocrine Society. The presenters will offer a review of the final guidelines for clinical practice, namely strategies for early diagnosis and management, including a narrative on who and how to treat, assessing patient complications and ongoing monitoring, and closing with a review of available and emerging therapeutic options to improve treatment selection.

Progressive Familial Intrahepatic Cholestasis (PFIC): Genetics, Treatment, and Management
Progressive Familial Intrahepatic Cholestasis (PFIC) comprises a group of rare, autosomal recessive genetic disorders marked by impaired bile formation, resulting in the hepatic accumulation of bile acids. If unrecognized or left untreated, PFIC can progress to severe liver disease and ultimately liver failure. Although uncommon, the condition’s severity—combined with evolving insights into its genetic underpinnings, diagnostics, and therapeutic options—highlights the need for targeted clinician education to support earlier diagnosis, evidence-based management, and improved patient outcomes.
Join us for an interactive panel discussion featuring real-world patient cases and expert-recommended strategies designed to address persistent clinician knowledge gaps and enhance clinical practice in PFIC care.

Recognizing Porphyria Attacks: When Severe Abdominal Pain Can Last up to 7 Days
This CME presentation was held as a satellite symposium at the 2025 Society of Hospital Medicine (SHM) Annual Converge Meeting.
Patients with certain inherited metabolic disorders often arrive in the emergency room/ hospital setting with porphyria-like attacks. To improve an understanding of AHP (acute hepatic porphyria) and to better differentiate it from other disorders that mimic symptoms associated with AHP, a broad differential diagnosis of the main acute presentations of acute porphyrias (including severe abdominal pain, extensive neuropathy issues, disabling respiratory symptoms, tachycardia, vomiting, and more) will be reviewed. Patient cases covering these neurovisceral acute attacks, with recommended strategies to for immediate patient treatment will be included.
Once you register for free on SHM's website, you will be able to view the presentation and claim CME credit.

Visualizing the Problem: Ocular Manifestations of Nephropathic Cystinosis
Nephropathic cystinosis is a rare genetic disorder that can cause ocular manifestations, kidney decline, small stature, muscle wasting, frequent thirst, and other symptoms. Join us for an exciting complimentary webinar as our expert panel provides an overview of the disorder , including an assessment of telltale signs and symptoms indicative of ocular cystinosis that manifest as a deposition of cystine crystals in the cornea, as well as kidney decline, small stature, muscle wasting, frequent thirst, as well as other symptoms. Optimal management approaches of evidence-based treatments will be reviewed using sample patient cases.
